One of the most striking findings in our longitudinal analyses at HealthSnap, spanning 25 million blood pressure data points across tens of thousands of patients, is how consistently and durably blood pressure improves when patients are supported monthly through Remote Patient Monitoring (RPM).
The figure below shows something we rarely see in real-world chronic disease management:
A steady, month-over-month decline in systolic and diastolic blood pressure that continues for 30 months.
Importantly, these analyses exclude patients who initiated new antihypertensive medications during this period. What you are looking at is pure behavioral, engagement-driven improvement—the effect of continuous monitoring, clinical feedback loops, and proactive care.
What Does This Mean Clinically?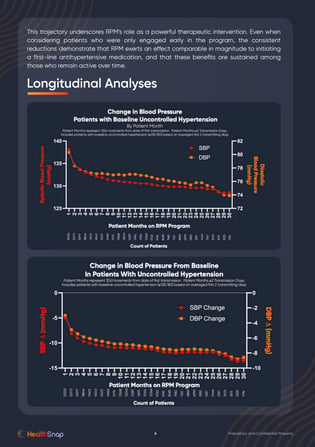
The early slope of improvement, often a 10–12 mmHg reduction in systolic blood pressure within the first 3–6 months, mirrors what we see when patients start a first-line antihypertensive medication such as a thiazide diuretic, ACE inhibitor, or calcium channel blocker.
But here’s the remarkable part:
The improvements don’t plateau. They continue.
RPM appears to exert a sustained behavioral and physiological effect long after traditional interventions typically level off.
How Does This Compare to Antihypertensive Medications?
Large randomized trials and meta-analyses consistently show that first-line antihypertensive medications, such as thiazide diuretics, ACE inhibitors, ARBs, and calcium channel blockers, reduce systolic blood pressure by approximately 8–12 mmHg on average.
What makes our findings striking is that patients entering the RPM program were not being initiated on a new antihypertensive medication at enrollment.
These are individuals already under the care of a provider, already on their established medication regimen, and managed in routine clinical practice.
Yet, despite no new medication being added, we observe reductions of similar magnitude—driven solely by the RPM intervention, which functions independently and exerts its own therapeutic effect through:
-
Continuous monitoring
-
Early detection and timely clinical adjustments
-
Behavioral reinforcement
-
Improved self-management and patient health literacy
-
Sustained engagement
-
Provider oversight supported by real-time data
In other words:
RPM is generating a medication-like effect in blood pressure reduction, even though no medication is being started.
This positions remote patient monitoring not simply as a workflow enhancement, but as a standalone therapeutic modality with population-level clinical impact.
Why This Matters: Risk Reductions Are Not Linear, They Compound
The landmark JAMA meta-analysis by Ettehad et al. (2016) found:
-
Every 5 mmHg reduction in SBP → ~10% reduction in major cardiovascular events.
-
Every 10 mmHg reduction → ~20% reduction.
Based on our observed average reductions in uncontrolled hypertension:
-
10–12 mmHg SBP improvement ≈ 20–24% reduction in major CV events.
These are population-scale numbers. When applied to Medicare beneficiaries, where hypertension is one of the highest-burden conditions, the implications are extraordinary.
Estimating Avoided Events and Medicare Savings
Using conservative assumptions from the Ettehad et al., JAMA 2016 meta-analysis—which demonstrated that a 10 mmHg systolic reduction lowers major cardiovascular events by ~20%, we can estimate the expected population-level impact in our 40,000 hypertensive patient cohort.
-
Among 40,000 hypertensive Medicare-aged patients, a 10–12 mmHg reduction in systolic BP would be expected to prevent ~800–1,200 major cardiovascular events per year, including myocardial infarctions, strokes, and heart-failure hospitalizations.
-
With the average cardiovascular hospitalization costing Medicare $20,000–$35,000, this corresponds to an estimated
~$16–$42 million in avoided annual spending in this 40,000 patient sample alone.
When scaled nationally across millions of eligible patients, RPM could represent one of the most cost-effective cardiovascular prevention strategies in the U.S. healthcare system.
Important Scientific Note
Our data represent observational, real-world evidence, not a randomized clinical trial.
As such, while the magnitude and consistency of improvement are compelling, the findings should be interpreted within the context of real-world variability and patient behavior.
However, what real-world evidence does offer is something clinical trials cannot:
A direct view into how patients improve in the context of everyday life, over years, not weeks.
The Takeaway
Hypertension is the leading modifiable risk factor for mortality worldwide. If a scalable, technology-enabled workflow can drive persistent, medication-independent, and population-level blood pressure reductions:
-
The clinical implications are enormous.
-
The economic implications for Medicare are even larger.
-
And the opportunity to redesign chronic care around continuous support, not episodic visits, is finally within reach.
This is what happens when longitudinal data, clinical workflows, and behavioral science intersect.
Remote Patient Monitoring is not a device, it’s a therapeutic intervention. And the real-world data are finally catching up to what clinicians see every day.
Tags:
RPM
Dec 8, 2025 3:22:27 PM


